Bien que petit, Les coins dentaires jouent un rôle irremplaçable dans la dentisterie réparatrice. Ils sont principalement utilisés pour la séparation des dents, stabiliser les bandes matricielles et façonner les bords des restaurations. Selon le matériau et la conception, Les performances cliniques et l'utilisation des coins varient. Dans cet article, Nous analyserons systématiquement les types de quartiers dentaires, leurs propriétés matérielles, leurs principales fonctions et leur application en remplissage et restauration.
1. Types de coins dentaires et de propriétés de matériaux
Quartiers dentaires en plastique
Matériel: Souvent fait de polypropylène médical (Pp), flexible.
Avantages:
- L'élasticité modérée réduit la pression sur les gencives.
- Peut être stérilisé à des températures élevées et convient à la réutilisation.
Désavantage:
- Support limité, pas adapté aux cas avec caries profondes ou des lacunes serrées.
Échantillon d'affichage:
- gardes de coins dentaires (GD-5675): avec trou avec rblade
trois taille: Grand / moyen / petit

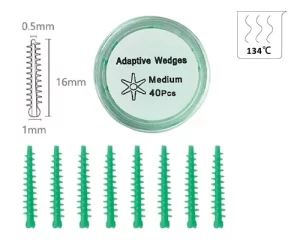
- cales adaptatives (GD-5677): avec un noyau en plastique intérieur ferme, couvert de silicone

- quartiers dentaires en résine (GD-5678): quatre taille, XS / S / M / L

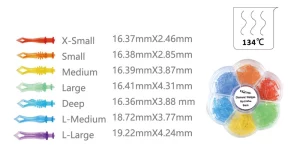
- quartiers de diamant (GD-5679): sept taille, X-Small / Small / Media

- Cales de Tulwar (GD-5680): trois taille, Petit / moyen / grand

Quartiers dentaires en bois
Matériel: principalement bouleau ou pin, stérilisé. Coins de bouleau avec une teneur en eau de 12% peut se développer jusqu'à 18.7% dans 30 minutes dans un environnement de liquide gingival. Cette propriété adaptative les rend particulièrement adaptés aux cas de récession gingivale chez les anciens patients. Cependant, Il faut prendre soin: La surexpansion peut entraîner une pression excessive sur la membrane parodontale, déclencher une sensibilité postopératoire.
Avantages:
- Naturellement absorbant à l'eau et gonflable, Meilleur ajustement à l'écart en peropératoire.
- Rigide, Convient pour le soutien à haute résistance aux cavités de classe II.
Désavantage:
- Non-reusable, La surexpansion peut causer de l'inconfort.
Échantillons Afficher:

Autres types
- Coin de métal: Rare, couramment utilisé pour la préparation complète de la couronne ou les scénarios de restauration spéciaux.
- Coin de silicone: doux et flexible, Convient aux restaurations esthétiques, mais plus coûteux.
2. Les trois fonctions principales du coin dentaire
Séparation des dents
- Sépare temporairement les dents voisines par 0.2-0.5 mm avec une force mécanique légère pour créer un espace de fonctionnement.
- Cela empêche la restauration de surplomber et restaure la forme naturelle des points voisins.
- Des études cliniques ont montré que l'utilisation appropriée des coins peut réduire le risque d'impaction alimentaire 60%.
Stabilisation de la bande matricielle
- Les quartiers dentaires peuvent aider à réparer la pièce de moulage, Empêcher la fuite du matériau réparateur et façonner le contour idéal.
- Cavité II Restaurations: la combinaison avec le Bandes matricielles La stabilisation est la solution classique.
- Cavity Class V Restorations: généralement en combinaison avec une plaque de moulure courbe.
Protection des gencives et hémostase
- Les cales dentaires peuvent offrir un certain degré de protection au-dessus des gencives.
- Une fois la cale dentaire insérée dans la dent, cela exercera une légère pression sur la gencive, réduire les saignements pendant l’opération.
3. Compétences d’application en remplissage et réparation
Comment choisir le bon coin
| Critères | Type de coin recommandé |
|---|---|
| Espace interproximal étroit | Cales en bois, il se dilate et s'emboîte après avoir été mouillé |
| Espace interproximal large | Coin plastique, coupe élastique |
| Résine légère | Cales en plastique transparent, faciliter la pénétration de la lumière |
| Remplissage d'amalgame | Cales en bois, il peut offrir un soutien plus fort |
Insérer l'angle et la direction
La cale dentaire doit être insérée obliquement dans l'espace interdentaire depuis le côté lingual ou buccal de la dent., et l'angle doit être contrôlé entre 30 ° et 45 °. L'objectif principal de cette conception d'angle est d'éviter le tissu des gencives, empêcher la compression directe ou le grattage de la gencive lors de l'insertion verticale, et réduire le risque de rougeur des gencives postopératoires, gonflement et saignement.
Contrôle de la profondeur d'insertion
Le haut de la cale doit être légèrement plus haut que le bord de la restauration d'environ 0,5 mm.. Cet espace réservé est conçu pour compenser le retrait lors du processus de durcissement des matériaux de remplissage ultérieurs. (comme la résine), garantir que le matériau peut adhérer étroitement au bord de la dent après durcissement et éviter la formation d'espaces pouvant conduire à des caries secondaires.
Précautions cliniques
Évitez une pression excessive sur les gencives: Pendant l'opération, la force d'insertion de la cale dentaire doit être contrôlée. Une pression excessive peut endommager la relation d'attache entre les gencives et les dents, ce qui peut provoquer une récession gingivale postopératoire. Les statistiques cliniques montrent que l'incidence de ces complications est d'environ 3% à 7%.
Positionnement précis de la position d'insertion: Si la cale dentaire est insérée dans une position décalée (comme être trop proche de la surface occlusale ou de la direction de la pointe de la racine), cela peut rendre les points de contact des dents adjacentes trop lâches, affectant ainsi la stabilité de la relation occlusale normale. Les patients peuvent rencontrer des problèmes tels qu'une morsure faible et une impaction alimentaire.
Cas réel: Réparation d'un défaut profond en forme de coin
Prenant comme exemple la réparation d'un défaut profond en forme de coin de la première prémolaire inférieure gauche, le fonctionnement spécifique et l'effet thérapeutique sont les suivants:
- Bilan préopératoire: Le patient était un adulte de 45 ans. Le défaut cervical de la première prémolaire inférieure gauche avait atteint la dentine profonde, accompagné de symptômes évidents de sensibilité au froid et à la chaleur. L'échelle visuelle analogique (SAV) a été utilisé pour évaluer le degré de sensibilité, avec une note de 6/10.
- Techniques de fonctionnement clés: D'abord, utilisez le Non. 00 ligne gingivale pour traitement de drainage gingival. Alors, insérez une cale de pin pré-humidifiée et laissez-la reposer pendant 15 minutes jusqu'à ce qu'il se dilate complètement pour élargir l'espace entre les dents. Suivant, la résine fluide est utilisée comme base, puis la résine 3M Z350XT est utilisée pour le remplissage en couches. Les cales doivent être conservées jusqu'à ce que la résine ait initialement durci avant d'être retirées pour éviter toute déformation du matériau pendant le processus de remplissage..
- Efficacité postopératoire: Le patient a été suivi pendant un an après l'opération. L'examen a montré que le taux d'intégrité de la restauration a atteint 98%, sans relâchement, décollement ou carie secondaire. Les symptômes de sensibilité au froid et à la chaleur du patient ont complètement disparu, et la fonction occlusale est revenue à la normale.
4. Critères d'achat des cales dentaires
Priorité de sécurité des matériaux
Normes de certification de base
Le matériau et le traitement de stérilisation de la cale doivent être conformes aux normes médicales professionnelles. Différents matériaux correspondent à des exigences de certification claires:
- Cales en plastique: Doit avoir la FDA (Administration des aliments et des médicaments des États-Unis) ou CE (Certification de sécurité des produits de l'Union européenne) certification polymère de qualité médicale. Le noyau doit éviter les substances nocives telles que les phtalates, qui peut migrer par contact et présenter des risques potentiels pour la santé. La certification de conformité est la base essentielle pour garantir la sécurité des matériaux.
- Cales en bois: Une EO complète (oxyde d'éthylène) un rapport de stérilisation doit être fourni, et le rapport doit clairement indiquer que la charge biologique est ≤10⁻⁶ (C'est-à-dire, la probabilité de survie microbienne après stérilisation ne dépasse pas un sur un million), s'assurer qu'il ne reste aucune bactérie pathogène avant utilisation pour éviter une infection croisée ou une inflammation postopératoire.
Points clés pour éviter les pièges des achats
Lors de l'achat, soyez prudent avec les produits de qualité non médicale et surtout rejetez-les “cales industrielles en bois” sans aucun marquage. La plupart de ces produits sont fabriqués à partir de restes de matériaux issus de la transformation industrielle et n'ont pas subi de traitement de qualité médicale.. Ils peuvent contenir des produits chimiques nocifs tels que le formaldéhyde. Lorsqu'il est utilisé, non seulement ils irritent facilement les tissus des gencives, mais peuvent également être absorbés par la muqueuse buccale, constituant une menace pour la santé du patient. De plus, il n'existe pas de normes unifiées pour leur taille et leur dureté, qui ne peut pas répondre aux exigences opérationnelles précises de la restauration dentaire.
Maximiser le taux d'ajustement de la taille
Lors du choix des cales, il est nécessaire de combiner les besoins cliniques réels et de maximiser le taux d'ajustement de la taille grâce à “évaluation préopératoire + réserve multi-spécifications”.
Avant l'opération, la taille de la cale requise doit être initialement déterminée en fonction de la largeur de l'espace interdentaire de la dent affectée (comme l'espace carieux interdentaire, espace de défaut en forme de coin) et la morphologie dentaire (comme les dents de lait et les dents permanentes, dents normales et dents inclinées).
Il est recommandé de s'approvisionner en plusieurs tailles de cales (comme mince, moyen, épais, ou des styles fins et épais pour des espaces dentaires spéciaux) pour éviter un mauvais ajustement dû à une taille unique insuffisante, ce qui peut affecter l'effet d'ouverture de l'espace ou provoquer une compression des gencives. Cela garantit qu'un modèle correspondant peut être trouvé pour différents cas, améliorer l’efficacité opérationnelle et la qualité de la restauration.
5. Conclusion
Bien que les coins dentaires soient de petite taille et semblent insignifiants, ils sont indispensables “rôles de soutien clés” dans les opérations de restauration dentaire. De la sélection des matériaux à une utilisation standardisée, un contrôle précis de chaque maillon n'est pas seulement la garantie fondamentale pour améliorer la stabilité de la restauration et réduire les complications postopératoires, mais peut également améliorer efficacement le diagnostic et l'expérience de traitement du patient et jeter les bases d'un bon pronostic à long terme.